What does melanoma look like on dogs

Melanoma Tumors in Dogs
Reviewed and updated for accuracy on April 29, 2019 by Dr. Hanie Elfenbein, DVM, PhD
Melanoma tumors in dogs demand immediate attention. In fact, early recognition of these malignant tumors of melanocytes (pigment-producing cells) is key. It can lead to more successful attempts at removal and identification of the grade or stage of cancer in order to direct treatment.
As a group, though, melanomas can be either benign or malignant. The risk of metastasis (spreading) for benign forms of melanoma is not very high, but these can be locally invasive, meaning there is harmful to normal tissue where the tumor forms.
Malignant melanomas in dogs, conversely, can metastasize (spread) to any area of the body, especially the lymph nodes and lungs, and present very challenging and dangerous prospects for the dog.
Heres what you need to know about melanomas in dogs.
Benign Melanomas in Dogs
Benign cutaneous melanomas in dogs are usually seen as round, firm, raised, darkly pigmented masses from 1/4 inch to 2 inches in diameter. They occur most often on the head, digits (toes) or back.
Malignant Melanomas in Dogs
Lymph-node swelling or enlargement may be a clinical sign of malignant spread of a melanoma in dogs. An abnormally concentrated amount of melanin (pigment) is often another hallmark of dog melanomas.
However, some melanomas do not display the characteristic darkly pigmented color of most melanomas. These are called amelanotic, and may be mistaken for other types of tumors unless evaluated by your veterinarian.
The location of the tumor may predict its severitytumors on the face, mouth, eye, feet and haired skin areas are especially concerning, though it is important to confirm that any lump is not cancer.
Diagnosis
A definitive diagnosis is made via microscopic analysis (histopathology evaluation by a specialist in veterinary pathology) of a small section of the growth.
This is also called a tumor biopsy. The examining pathologist usually will grade the specimen according to how actively the cells are replicating. This gives an approximation of how likely the growth is to invade and spread.
If an entire growth is removed, the pathologist can report on the tissue's grade as well as any evidence that parts of the tumor may not have been thoroughly excised by the surgeon.
Your veterinarian will also want to examine your pet for metastasis by taking X-rays of the chest and tissue samples from lymph nodes. This process, called staging, helps your veterinarian select the right types of treatment and gives you important information about your pets prognosis.
Treatment
Treatment of melanomas in dogs is best provided by surgical excision of the tumor and nearby surrounding tissue. Localized tumors in a dog may be completely removed with the patient being cured.
However, if a malignant melanoma has had the opportunity to spread to distant areas of the body, the prognosis for the dog is not favorable.
Chemotherapy has been performed with marginal success, though complete remissions of metastatic melanoma cases are rare. Fortunately, most cutaneous (skin) melanomas are benign; nevertheless, individual growths should be evaluated carefully, as any given melanoma may become malignant.
There is also a melanoma vaccine for dogs. Unlike most vaccines, this therapy does not prevent melanoma tumors from forming, but rather helps the body rid itself of any remaining melanoma cells after the tumor has been removed.
This can be helpful when the tumor is in a place where your surgeon is unable to remove the entire mass, such as the mouth, eye and toes.
Case Presentation of Melanoma in Dogs
A Golden Retriever was presented for routine vaccinations. The attending veterinarianas part of the pre-vaccination physical examnoticed an abnormal, darkly pigmented, raised tissue mass at the lateral edge, or the dog's right corneal-scleral junction.
The suspicious mass was creating a slight deviation in the smooth surface of the cornea and seemed to be invading both the sclera (white area of the eyeball) and the cornea.
Because the veterinarian suspected that the mass was a melanoma, referral to a specialist in Veterinary Ophthalmology was done. Dr. Sam Vainisi of the Animal Eye Clinic in Denmark, Wisconsin, evaluated the 4-year-old Golden Retriever and recommended surgery.
Using a CO2 laser, the growth was excised. Because of the depth and diameter of the growth, as well as the unusual location, Dr. Vainisi performed a frozen-tissue, corneal-scleral graft with healthy tissue from the clinic's eye bank to fill in the defect.
The tissue graft was carefully sutured into the surgical site. Topical and oral dog antibioticsand an anti-inflammatory medication were used after the surgery, and healing of the surgical site was uneventful.
The photos below display the melanoma prior to the surgery and six months after. Annie, the patient, is healthy and active and is expected to have no visual impairment as a consequence of the tumor. Thanks to the specialist's careful evaluation and surgical excision of this melanoma, Annie is expected to have no further problems with the eye.
Benign Melanoma in the Eye of a Dog
(click on an image to see the close-up view)
Two views of a dark, raised mass of six month's duration at the corneoscleral junction in a Golden Retriever.
Two views of the healed surgical site, six months after surgical excision and with tissue transposition.
If you discover a darkly pigmented, raised, thickened growth anywhere on your dog, be sure to have your veterinarian evaluate it. Keep in mind that pigmented (black) areas of the skin are common in dogs (and cats), especially in the tongue, gum and eyelid tissues. These darkened areas may be completely normal for that individual.
However, if any darkly pigmented areas are actually raised above the normal surface or seem thickened, ulcerated or inflamed, an exam is indicated. Any new areas of pigmented or raised tissue should be evaluated by your veterinarian.
Featured Image: iStock.com/miodrag ignjatovic
Malignant Melanoma in Dogs A Colorful Canine Cancer
With my bald head, Im keenly aware of my risk for skin cancer, specifically malignant melanoma. Unfortunately, our canine companions can develop this cancertoo. This cancer is quite aggressive, so I wanted to share information with pet parents to raise awareness. Please consider sharing with other dog parents you know. Happy reading!

Malignant Melanoma What is it?
Malignant melanoma are tumors of pigment-containing cells called melanocytes. As such, these tumors are commonly found where there is pigment skin, hair, and the eyes. Veterinarians dont currently know what triggers malignant melanoma to form. Some have suggested trauma, possibly excessive licking of a particular body part, and even stress may stimulate cells to randomly multiply. By doing so, there is the potential random mutations that result in the formation of cancer cells. Interestingly, sun exposure does not appear to induce melanoma in our canine companions. The most common forms of malignant melanoma:
- Cutaneous (5-7% of canine skin tumors)
- Oral (30-40% of canine oral tumors)
- Digits (nail bed, footpad)

Oral malignant melanoma in a dog. Photo courtesy of VetPedia
Malignant melanoma can also occur in the eye, gastrointestinal tract, and mucocutaneous junctions. This cancer typically occurs in older dogs, and some breeds are over-represented:
- Scottish terriers
- Dachshunds
- Cocker spaniels
- Poodles
- Golden retrievers
Malignant Melanoma What does it look like?
The oral and skin formsare typically highly pigmented (brown to black), raised masses. Interestingly, approximately one third of melanoma are completely devoid of dark discoloration and appear like normal pink/tan skin. They can be found in the gingiva/gums (42-63%), lips (15-33%), hard & soft palate (10-16%), and tongue (1.5-3.3%). Oral malignant melanomas are often associated with halitosis (bad breath), ptylasim (excessive drooling), dysphagia (difficulty swallowing), and abnormal breathing noises (i.e.: stertor, stridor). Malignant melanoma of the digit/toe typically causes swelling of the involved toe, as well as loosening of the associated nail and lameness on that leg.
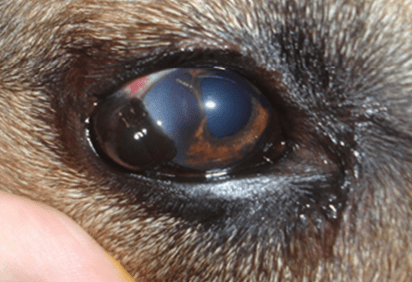
An ocular malignant melanoma in a dog. Photo courtesy of Dr. A Nishiya
Malignant Melanoma How is it diagnosed?
Early diagnosis is essential. In a previous blog, I have emphasized the concept of #SeeSomethingDoSomething initiated by board-certified veterinary oncologist, Dr. Sue Ettinger (DrSueCancerVet). For example, any skin mass that has been present for more than one month and/or is larger than the size of a pea should be evaluated by a veterinarian. This evaluation should include either aspiration or biopsy of the mass. No veterinarian can simply look or touch a skin mass and know what it is. As Dr. Ettinger advocates, #WhyWaitAspirate!
An aspiration involves inserting a vaccine-sized needle into the tumor and removing some cells. Aspirating skin masses does not typically require sedation, but sampling from an oral often requires sedation. The aspirated cells should be evaluated by a board-certified veterinary clinical pathologist to obtain a definitive diagnosis. The evaluation of the aspirated cells is called cytology. Occasionally, cytology is not diagnostic. In such cases, a surgical biopsy is required to obtain a definitive diagnosis.
Once a malignant melanoma has been confirmed, some additional non-invasive testing is recommended to determine how involved the body is with the cancerous process. These tests include:
- Complete blood count (CBC) a non-invasive blood test that provides information about red blood cells, white blood cells, and platelets
- Serum biochemical profile (CHEM) a non-invasive blood test that yields information about liver and kidney function, as well as electrolytes (i.e.: sodium, potassium), and certain gastrointestinal enzymes
- Urinalysis (UA) a non-invasive urine test that helps assess kidney function, and screen for inflammation and infection in the lower urinary tract
- Chest radiographs / x-rays (CXR) images of the heart lungs to look for evidence of metastasis / spread of cancer
- Abdominal sonography (AUS) a non-invasive imaging test of the abdomen to screen for metastasis in internal organs like the spleen and liver
- Aspiration of the local lymph node Like the test perform to diagnose melanoma, this minimally invasive test screens for melanoma cells that have metastasized to the lymphatic system
The above described testing is called staging, and staging helps veterinarians determine how advanced a pets cancer is. Most importantly, the results of staging diagnostics can provide information about a pets prognosis, and thus can be quite helpful to both veterinarians and pet parents. For example, oral malignant melanoma has four stages:
- Stage I: Primary tumor <2 cm in diameter
- Stage II: Primary tumor 2 to <4 cm in diameter
- Stage III: Primary tumor larger than 4 cm in diameter and/or metastasis to lymph node
- Stage IV: Distant metastasis (i.e.: chest, abdomen) present
Malignant Melanoma How is it treated?
Malignant melanomamay be treated with surgery, radiation therapy, and chemotherapy. I like to think of treatment as having two components:
- Local control
- Systemic control
To achieve the first goal of local control, aggressive surgery is indicated. Such an intervention allows in most cases removal of the tumor from its current location. For example, skin masses should be removed whenever possible. Amputation of an affected digit is recommended. Oral surgery may involve removal of part of the jaw. This is understandably an unsettling proposition for many pet parents. Happily, more than 85% of patients undergoing such surgeries have satisfactory functional and cosmetic outcomes. The reported median survival times oral malignant melanoma following surgery are:
- Stage I: 17-18 months
- Stage II: 5-6 months
- Stage III: 3 months
- Stage IV: 1 month
Dogs with digit malignant melanoma without lymph node involvement or distant metastasis treated with toe amputation have a reported median survival time of ~12 months. In previous studies, approximately 42-57% were alive at one year and 11-13% were alive at two years. Pet parents are encouraged to collaborate with board-certified veterinary surgeons to ensure the most appropriate surgical approaches are taken to achieve local control.

Pre-surgical picture of malignant melanoma of a digit in a dog. Photo courtesy of Dr. P Bergman
Unfortunately, surgery is not an option for some patients. In others, malignant melanoma cant be completely excised via surgery due to their location. For these patients, radiation therapy is a helpful therapeutic adjunct. Radiation therapy has been associated with partial and complete response rates of 25-30% and 53-69% respectively. Reported median survival times were 5-8 months.
Once local control of malignant melanoma has been achieved as best as possible, effort should be put forth to prevent (or at least try to slow down) the spread of the cancer. Such an effort is also indicated for patients who are not candidates for surgery and for those who had malignant melanoma that could not be completely removed with surgery. The biggest question is how to achieve this goal of systemic control. The use of chemotherapy to achieve systemic control is controversial. Chemotherapy treatments may include:
- Carboplatin
- Cisplatin
- Dacarbazine
- Melphalan
- Doxorubicin
- Toceranib
- Non-steroid anti-inflammatory drugs (NSAIDs)
To date, response rates to chemotherapy have been low and inconsistent. Perhaps most importantly, there is little evidence chemotherapy improves survival time. Pet parents will likely find it helpful to consult with a board-certified veterinary oncologist to determine if chemotherapy is appropriate for their fur babies.
Malignant Melanoma Are there any new treatments?
A novel treatment using a special vaccine (Oncept) has been approved to treat dogs with Stage II and III oral malignant melanoma after achieving local and regional control with surgery and/or radiation therapy. The vaccine has also been used to treat patients with malignant melanoma of the digits. The vaccine contains DNA to leads to the production of a unique protein called human tyrosinase. Tyrosinase is involved with pigment (melanin) formation in normal pigment cells and melanoma. When human tyrosinase is injected into a dog, the immune system identifies it as a non-dog substance. It is a foreign substance, and the immune system responds accordingly. Human and dog tyrosinase molecules are quite similar. Therefore, the immune response that attacks the injected human tyrosinase also attacks dog tyrosinase in malignant melanoma.
A multi-centered study showed survival time in dogs with Stage II or Stage III oral malignant melanoma with local/regional control that was received the vaccine was significantly longer than those not treated with the vaccine. In fact, the median survival time could not be determined because too few died of their died before the end of the study. Dogs with digital malignant melanoma treated with both surgery (for local control) and the melanoma vaccine had a median survival time of 476 days. The presence of metastasis was associated with a worse outcome 533 days without and 105 days with metastasis. The melanoma vaccine is only available through board-certified veterinary oncologists and internal medicine specialists.
The take-away message about malignant melanoma in dogs
Malignant melanoma is an aggressive cancer in dogs that most commonly occurs in the oral cavity, skin, and digits/toes. Early identification followed by initial aggressive local/regional control with surgery and/or radiation therapy is of paramount importance. Adjuvant therapies, including treatment with the melanoma vaccine, may confer a survival benefit.
To find a board-certified veterinary oncologist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
Wishing you wet-nosed kisses,
cgb